Where is the T3 Coming From? – The most important question in thyroidology.
We measure TSH, fT3 and fT4 in the blood. Blood is the ‘intermediate space’, it conveys hormones from the primary space (thyroid or tablets) to the active space (the receptors in the cell nucleus). Thyroid status is determined by T3 saturation at the receptors. The current view is that we can’t know tissue T3 levels because we can’t directly measure them. This approach fails to address important issues: –
- Many patients are hypothyroid with normal blood hormone levels
- Restoring normal blood hormone levels is not sufficient to cure all cases of hypothyroidism.
We know about ‘T3’ and other molecules because particle physicists detect and measure atomic particles. Endocrinology must adopt similar initiatives in order to understand what happens to thyroid hormones within tissues.
We can’t directly measure intracellular T3 levels, but we can use our understanding of thyroidology to interpret TFTs in a way that gives an indication of tissue hormone levels. We must look at where the T3 is coming from and to do so we need to understand deiodinases, specifically T4 to T3 conversion. For a detailed understanding refer to ‘Metabolism of Thyroid Hormone’ in Thyroid Disease Manager (register for free) and the content of Bianco Lab, both of which are listed under Resources. For simplicity, we concentrate on T4 to T3 conversion.
T3 comes from various sources: –
- The Thyroid – Secretes T3 and converts T4 to T3
- From Tablets – T3 in Liothyronine and natural desiccated thyroid (NDT)
- Peripheral tissues – Type-1 deiodinase
- Peripheral tissues – Type-2 deiodinase
Deiodinases
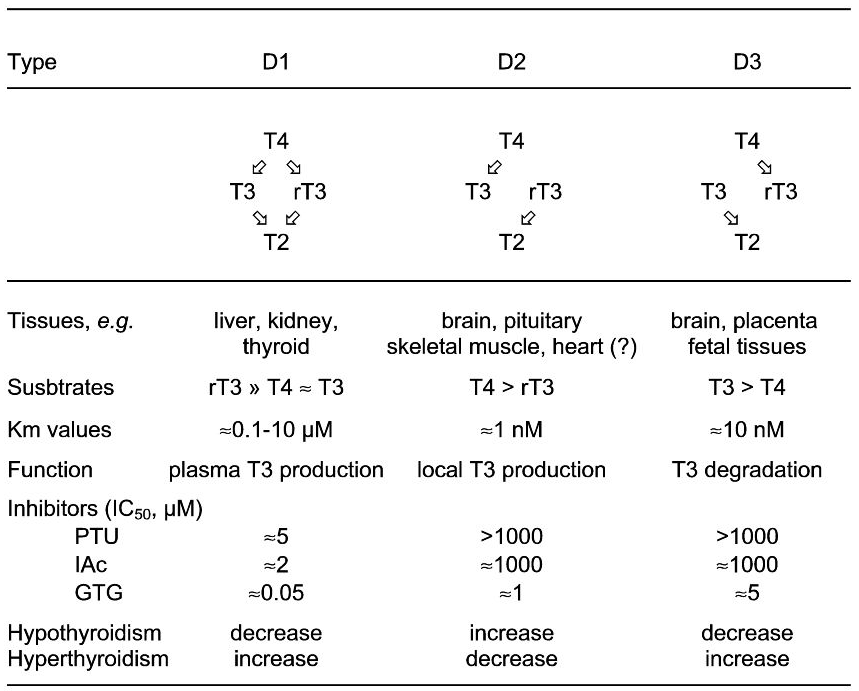
There are three deiodinases, Type-1, Type-2 and Type-3 referred to as D1, D2 and D3. (See this helpful diagram from thyroidmanager)
7. TRADEMARK AND COPYRIGHT INFORMATION ENDOCRINE EDUCATION, INC., THYROID DISEASE MANAGER, AND THYROIDMANAGER are trademarks of ENDOCRINE EDUCATION, INC. The information available through the website is the property of ENDOCRINE EDUCATION, INC. and is protected by copyright. Information received through the site may be displayed, reformatted and printed for your personal, non-commercial use only. You agree not to reproduce, retransmit, distribute, disseminate, sell, publish, broadcast or circulate the information received through the website to anyone without permission from ENDOCRINE EDUCATION, INC. Any copy made of information obtained through the site must include the copyright notice.
- D1 converts T4 -> T3, T4 -> rT3 usually in equimolar amounts. D1 is expressed in the liver, kidneys and thyroid. D1 is localized in the plasma membrane of the cell and provides plasma T3, it also mitigates the effects of thyrotoxicity by converting half the T4 to rT3. D1 activity increases in hyperthyroidism and reduces in hypothyroidism.
- D2 converts T4 -> T3. It is expressed in the pituitary, brain, brown fat (BAT), skeletal muscle and the heart. D2 is localized in the endoplasmic reticulum, close to the cell nucleus. D2 is responsible for local T3 levels, it is also the major source of circulating T3. Peripheral D2 activity decreases in hyperthyroidism and increases in hypothyroidism – the opposite of D1 and D3.
- D3 converts T4 -> rT3, T3 -> T2. It is expressed in the brain, placenta and foetal tissues. D3 activity increases in hyperthyroidism and decreases in hypothyroidism. D3 prevents excess T3 levels.
The deiodinases respond in complex ways to thyroid hormones and other influences to maintain local and circulating T3 levels. For example, D2 activity in brown adipose tissue increases dramatically during cold exposure. D2 activity in peripheral tissues decreases as T4 levels rise but the hypothalamus and pituitary are unique in that their D2 activity does not vary in this manner. This makes sense, the hypothalamus and pituitary measure circulating fT3 and fT4 levels. Deiodinase in other tissues responds to circulating hormone levels and local requirements.
Which T3 Matters?
Tissues such as the brain and skeletal muscle rely on D2 activity to regulate local T3 levels.
Most T3 comes from peripheral deiodinase of T4 with D2 being the major source. D2 activity increases as thyroid hormone levels fall. In hypothyroid scenarios the rate of T4 to T3 conversion increases, as we saw in McDermott’s Figure 1. This maintains not only circulating T3 levels but also crucially local T3 levels in tissues such as the brain which are highly dependent upon D2 activity.
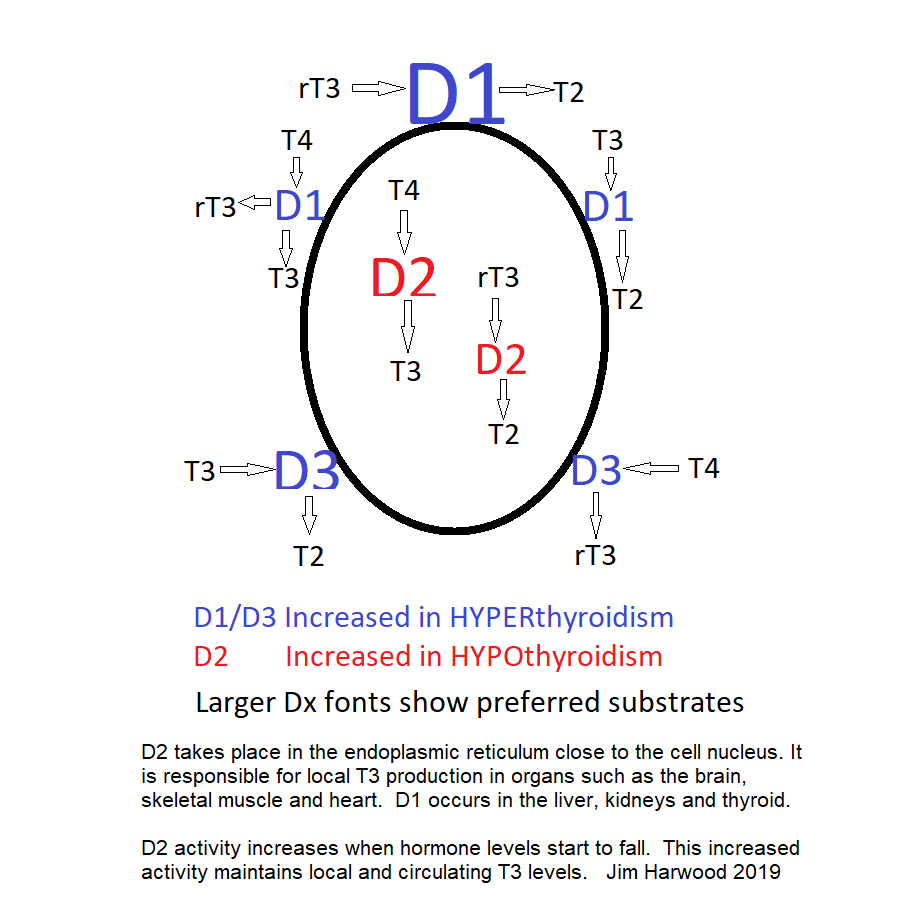
The diagram below shows how deiodinases control local and circulating T3 levels. Larger fonts indicate preferred substrates, i.e. which hormone the enzyme prefers to work on. D1 and D3 takes place near the cell membrane whereas D2 is located close to the cell nucleus. If you find the detail a bit too much, just look at the D2 enzyme. D2 activity increases as thyroid hormone levels fall thus maintaining stable T3 levels – at least until T4 levels have fallen too low.
D2 is especially important in the brain. In rats up 80% of cerebral cortex T3 comes from D2 converting T4 to T3.
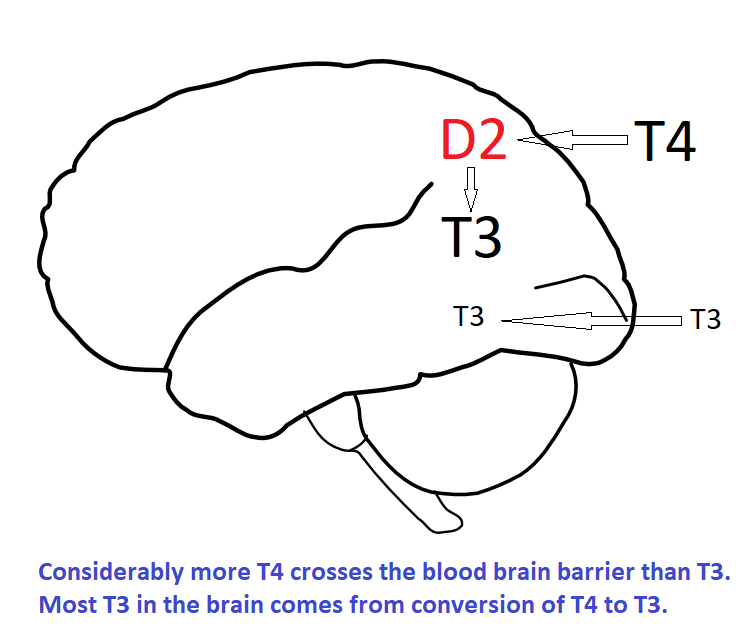
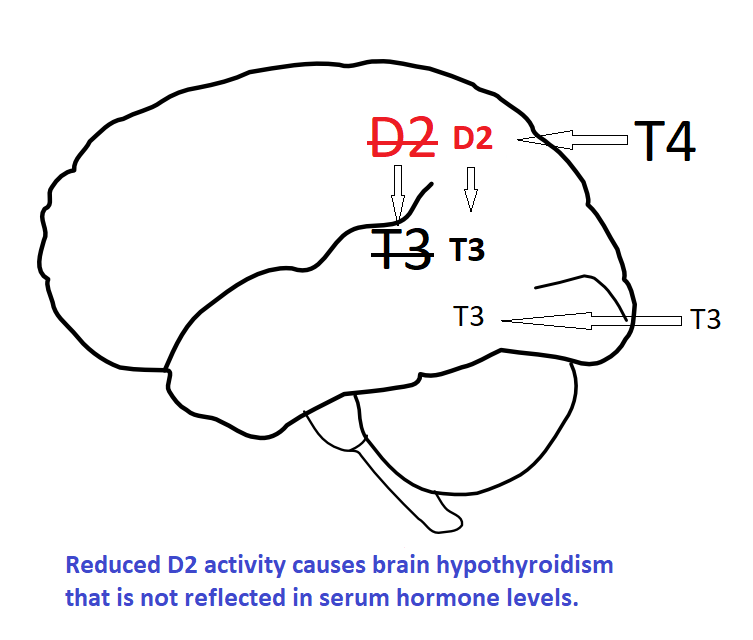
Consider what happens if D2 activity is reduced and sufficient levothyroxine / liothyronine prescribed to restore normal serum levels. The reduced D2 activity reduces T3 levels within the brain causing a form of brain hypothyroidism that cannot be detected by blood tests. Restoring normal brain T3 levels requires supra-physiological blood T3 levels.
We have seen that ‘D2T3’ is rather special now let’s see why Type-2 Deiodinase (D2) is Crucial.