Since it was written a few months ago this topic has become outdated. The information is correct but more recent studies have shown more typical results, perhaps due to advances in treatment. Until there is an update please bear in mind that later studies may contradict some of the earlier ones cited here.
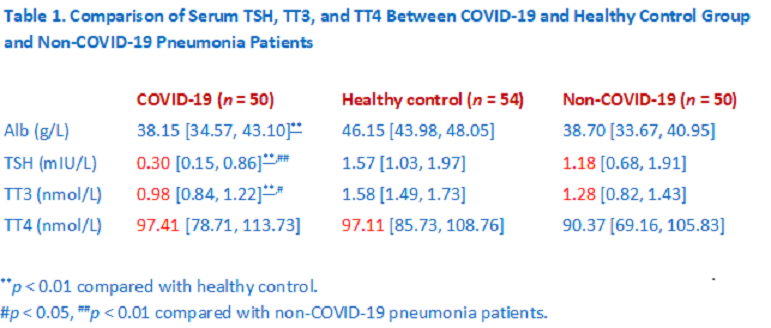
A recent study found remarkable effects of COVID-19 on the hypothalamic pituitary thyroid (HPT) axis presenting with a unique form of non-thyroidal illness (NTI). TSH, TT3 and TT4 returned to normal after recovery.
A Retrospective Study Min Chen, Weibin Zhou, and Weiwei Xu. Thyroid. ahead of print
http://doi.org/10.1089/thy.2020.0363
This study has two striking features: –
- Low TSH (0.30 mIU/L) is associated with normal T4 levels.
- The fall in TT3 exceeds normal thyroidal output indicating altered peripheral deiodinase.
Why is this study important for thyroid patients?
TSH is a group of isoforms which regulate deiodinase and secretion. TSH bioactivity and quantity are controlled by feedback from fT3 and fT4 and feedforward by TRH.
T4 is normal in COVID-19 even though TSH is low. There may be isoform specific effects which present a unique opportunity to investigate how TSH isoforms regulate deiodinase and secretion.
A normal T4 with a TSH of 0.30 mIU/L raises questions of how informative TSH immunoassays are. How should they be interpreted? Can better assays be developed?
Better understanding of TSH isoforms will improve diagnosis and could identify patients who will benefit from combined L-T3 / L-T4 therapy.
Why is this study important for COVID-19 patients?
Low TSH and low T3 with normal T4 may be a signature of severe COVID-19 – a distinct form of NTI. Perhaps COVID-19 has a unique TSH isoform profile that could identify COVID-19 patients who will need critical care.
Some COVID-19 patients have signs and symptoms of hypothyroidism and post infective NTI.
Similar sequalae occur in other SARS infections. An understanding of how COVID-19 affects the HPT axis would enable optimal care of COVID-19 patients and future SARS patients.
Another study finds COVID-19 NTI is associated with disease severity
Another study Zou R, Wu C, Zhang S, et al. Euthyroid Sick Syndrome in Patients With COVID-19 Front. Endocrinol., 07 October 2020. doi.org/10.3389/fendo.2020.566439 found a significant association between NTI and COVID-19 disease severity.
Confounding factor – Thyrotoxicosis in some COVID-19 patients
Studies have also found thyrotoxicosis in patients with COVID-19 infection: –
Lania A, Sandri MT, Cellini M, Mirani M, Lavezzi E, Mazziotti G. Thyrotoxicosis in patients with COVID-19: the THYRCOV study. Eur J Endocrinol. 2020;183(4):381-387. doi:10.1530/EJE-20-0335 Thyroid function was evaluated on the first day of hospitalization and thyroid hormones measured in those with abnormal TSH values. Overt thyrotoxicosis (low TSH, elevated fT3 or fT4) was found in 31 / 287 patients and accompanied by atrial fibrillation in 10 patients. There were no local signs or symptoms of subacute thyroiditis. Patients (with abnormal TSH) tended to have normal serum fT3 levels and none of those with a suppressed TSH had a low fT3.
Muller I, Cannavaro D, Dazzi D, et al. SARS-CoV-2-related atypical thyroiditis. Lancet Diabetes Endocrinol. 2020;8(9):739-741. doi:10.1016/S2213-8587(20)30266-7 Thyroid function was evaluated on average two days after admission. fT3 and fT4 were measured if TSH < 0.45 mIU/L (0.28-4.3). Patients with low TSH and/or elevated fT4 were classified as ‘thyrotoxic’. Of 85 patients admitted to the high intensity of care unit 13 were classified as ‘thyrotoxic’ with a mean fT4 18.7 (10.3 – 21.9) and fT3 2.9 (3.1 – 7.7).
Alessandro Brancatella, Debora Ricci, Nicola Viola, Daniele Sgrò, Ferruccio Santini, Francesco Latrofa, Subacute Thyroiditis After Sars-COV-2 Infection, The Journal of Clinical Endocrinology & Metabolism, Volume 105, Issue 7, July 2020, Pages 2367–2370, https://doi.org/10.1210/clinem/dgaa276 An interesting case of a woman who had a normal thyroid blood test one month earlier. Fifteen days after testing positive for SARS-Cov-2 she developed fever and neck pain radiating to the jaw. Her TSH was very low and fT3 / fT4 elevated.
Alessandro Brancatella, Debora Ricci, Daniele Cappellani, Nicola Viola, Daniele Sgrò, Ferruccio Santini, Francesco Latrofa, Is Subacute Thyroiditis an Underestimated Manifestation of SARS-CoV-2 Infection? Insights From a Case Series, The Journal of Clinical Endocrinology & Metabolism, Volume 105, Issue 10, 1 October 2020, dgaa537, https://doi.org/10.1210/clinem/dgaa537 This study describes four patients who developed subacute thyroiditis 16 to 36 days after resolution of COVID-19. They had neck pain radiating to the jaw with low TSH and elevated fT3 / fT4.
MattMattar SAM, Koh SJQ, Rama Chandran S, Cherng BPZ. Subacute thyroiditis associated with COVID-19. BMJ Case Rep. 2020 Aug 25;13(8):e237336. doi: 10.1136/bcr-2020-237336. PMID: 32843467; PMCID: PMC7449350. Ten days into his illness this patient developed neck pain and sinus tachycardia with a supressed TSH and very high fT3 and fT4.
Mari Des J. San Juan, Mary Queen V. Florencio, and Mark Henry Joven (2020) SUBACUTE THYROIDITIS IN A PATIENT WITH CORONAVIRUS DISEASE 2019. AACE Clinical Case Reports: November/December 2020, Vol. 6, No. 6, pp. e361-e364. The patient presented with anterior neck pain and swelling which started seven weeks earlier. She was diagnosed with subclinical hyperthyroidism which resolved after a month. She developed primary hypothyroidism eight weeks later.
COVID-19 can present with a form of NTI with a low or normal TSH, low fT3 and normal fT4. On the other hand, some patients develop subacute thyrotoxicosis with elevated fT3 and fT4. COVID-19 patients have lower T3 / T4 ratios than other forms of NTI and thyrotoxicosis. These two conflicting presentations have the potential to confound study results. A study of COVID-19 in patients who do not have a thyroid would reveal the peripheral effects of COVID-19 on thyroid hormone status.
Call for a study of TSH isoforms in COVID-19 patients
A study of thyroid function tests (TFTs) in athyreotic COVID-19 patients receiving levothyroxine monotherapy would characterise NTI in COVID-19 patients. It could reveal the effects on the HPT axis and peripheral deiodinase. Comparison with TFTs taken after recovery might elucidate the link between TSH isoforms and deiodinase. Such a study should exclude patients with elevated TSH receptor antibodies.
TSH is a package of messages (isoforms). Our current approach is analogous to weighing a letter rather than reading its contents. COVID-19 offers an unrivalled opportunity to discover the roles of TSH isoforms in NTI.