We’ve seen that T4 promotes cancer, but does it happen in real life? We look at serum T4 in cancer studies that exclude subjects who have had or develop cancer within a few years of the blood test. We first look at T4 and cancer in the general population. These studies will have confounded results because some people with abnormal thyroid test results will receive treatment. Their T4 level as recorded in the study may be quite different to the level throughout the study period. However, normal and so called ‘subclinical’ results are less likely to prompt therapy and so perhaps be more informative.
We’ve seen that the αvβ3 Receptor proliferates cancer by multiple mechanisms. It is important to look at both cancer risk and mortality because it is possible that T4 makes cancer more deadly independent of any effect on risk.
The Rotterdam Study
The ‘Rotterdam Study’ monitored 14,926 subjects aged over 45 years from 1990 until the end of the study on January 1, 2012. Most of the subjects were not on any form of thyroid medication, the results were similar when those on thyroid medication were excluded from the calculations. The graph below shows how the risk of solid cancer is higher for higher fT4 levels. The p-values are very small indicating that the results are reliable.
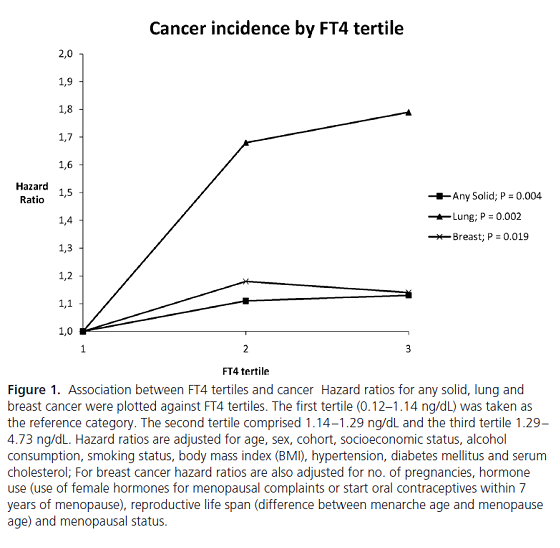
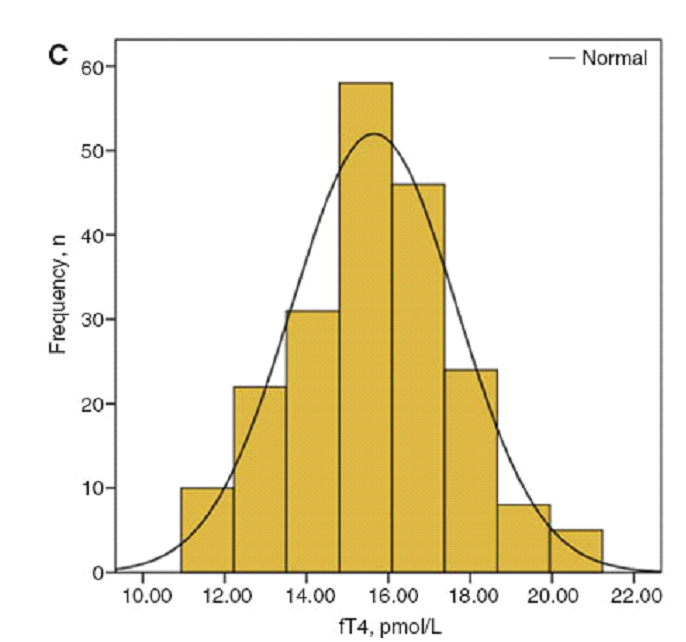
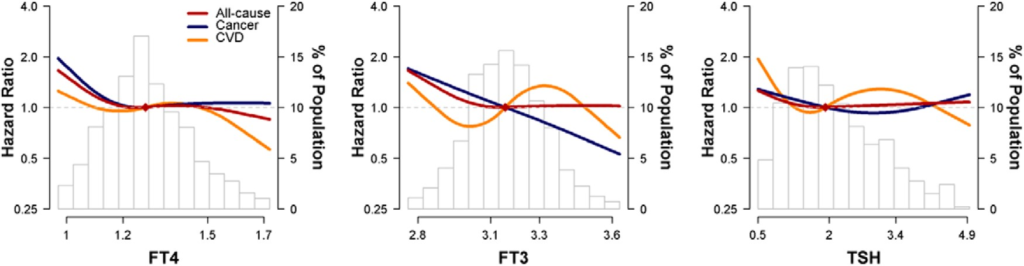
These results are for ‘tertiles’, the entire study population is split into three equal groups. However, most of the population clusters around the middle of the reference interval as can be seen in the graph below. The area of the first and last three bars is similar to the central two bars. Indeed, two thirds of the population fall in the second and third tertiles and so they are a better reflection of average risk, a better baseline. The graph suggests that low fT4 or even hypothyroidism is protective against cancer, especially lung cancer.
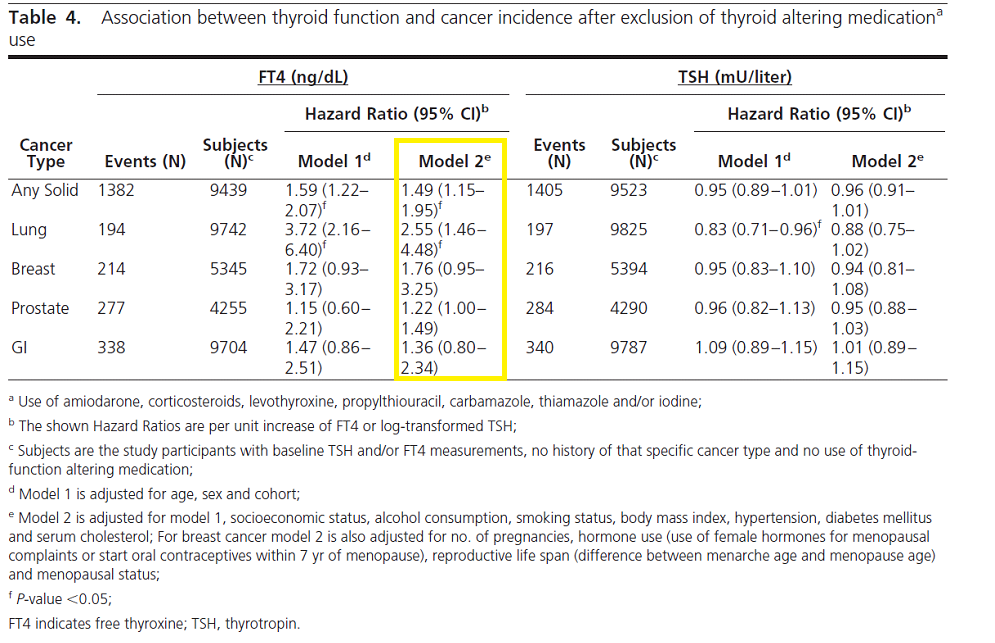
If we look at the FT4 column in Table 4 (model 2e) from the Rotterdam study we see the Hazard Ratios (HR) for the general population excluding people on thyroid medication. The HR for Any Solid cancer is 1.49. We need to interpret this, it’s a rather difficult concept. Comment b tells us that the FT4 Hazard ratio is ‘per unit increase’. This means an increase FT4 from e.g. 1.0 ng/L to 2.0 ng/L increases the risk of any solid cancer by 49%. 1 ng/L corresponds to 12.872 pmol/L. For example, if fT4 increases from 18.0 to 22.0 there is a 15% increased risk of a solid cancer. The assays used in this study had an fT4 reference interval of 11-25 pmol/L so increasing fT4 from 18.0 pmol/L to 22.0 pmol/L is typical of the difference between fT4 levels of the general population as compared to those on levothyroxine monotherapy. 15% represents the increased risk of getting cancer not mortality risk.
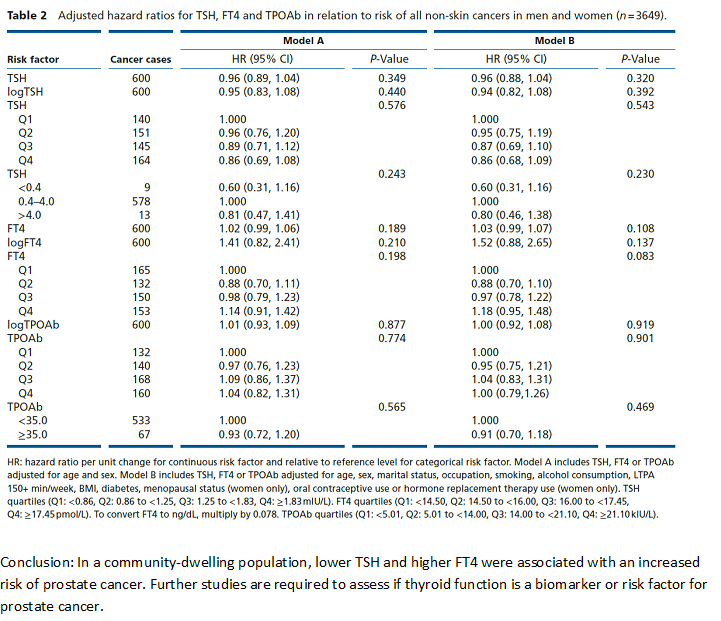
A Study of 3649 Subjects (600 cancer cases) With a 20-year Follow-up.
The next study was smaller with a younger age group and longer follow-up (20 years vs. 10.4 years in the Rotterdam study). This study found no association of TSH, fT4 or TPOAb with all non-skin cancer events. It found a small association with prostate cancer for TSH and fT4. It’s possible this study didn’t have the sufficient power to detect links and perhaps the results were confounded by more people developing thyroid disease during the long follow-up time.
A Large Study With a Subanalysis Which Excluded Subjects Who Took Thyroid Medication During the Study Period.
The following study found elevated fT4 was associated with increased cancer risk in the younger < 50 age group whist clinical hyperthyroidism was associated with lower cancer risk in the older >= 50 group. Bear in mind that cancer is much more common in older people and people with borderline hormone levels are likely to receive therapy during the study confounding the results. This study also did a subgroup analysis excluding anyone who received thyroid altering medications DURING the study period. As shown in Supplemental Table 9 below there was no consistent link between fT4 and overall cancer risk. There was a link between fT4 and lung cancer and an inverse link to colorectal cancer. The results for fT4 outside its reference interval may fail to reach statistical significance due to the small number of cases.
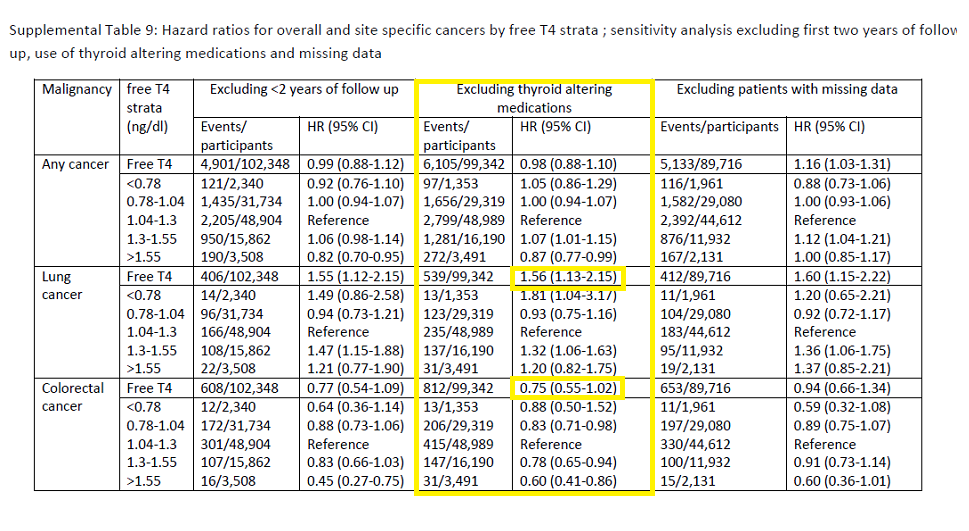
(The full paper is available to download from the ResearchGate website. The Supplementary Materials are available for free from the Journal website. The image link above downloads a pdf copy of the table)
Mortality Risk in Euthyroid Individuals
A study in a younger group with a relatively short follow-up of 4.3 years found fT4 was inversely associate with all-cause mortality and fT3 inversely associated with cancer mortality. Higher fT3 and fT4 seem to be safer. This was a well conducted study which excluded subjects with abnormal TSH, fT3, fT4, any diagnosis of thyroid disorders and cancer within the first three years.
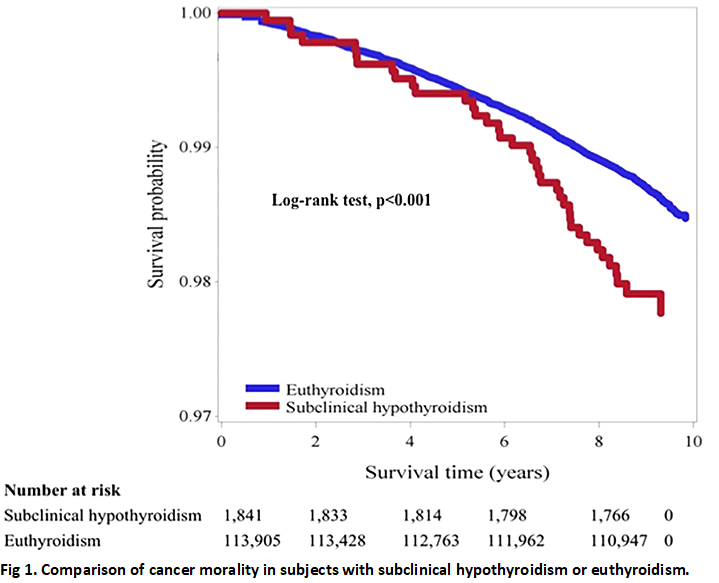
Cancer Mortality in ‘Subclinical Hypothyroidism’
The graph below shows that subjects with ‘subclinical hypothyroidism’ have lower cancer survival than euthyroid individual. This is the opposite of what we have seen in some studies so far, this study found that an elevated TSH and slightly lower T4 levels (93.1 nmol/L vs. 99.9 nmol/L) were associated with higher mortality. The graph is of unadjusted data but even when adjusted for e.g. age, smoking etc. ‘subclinical hypothyroidism’ had a cancer mortality relative risk (RR) of 1.61.
This was a study over a period of 10 years. The study excluded subjects receiving thyroid medication at baseline and fT4 was not measured. There were no follow-up blood tests and they did not know if any of the patients received thyroid treatment during the study period. This is relevant as the subjects were recruited from private screening clinics and so were more likely to be treated.
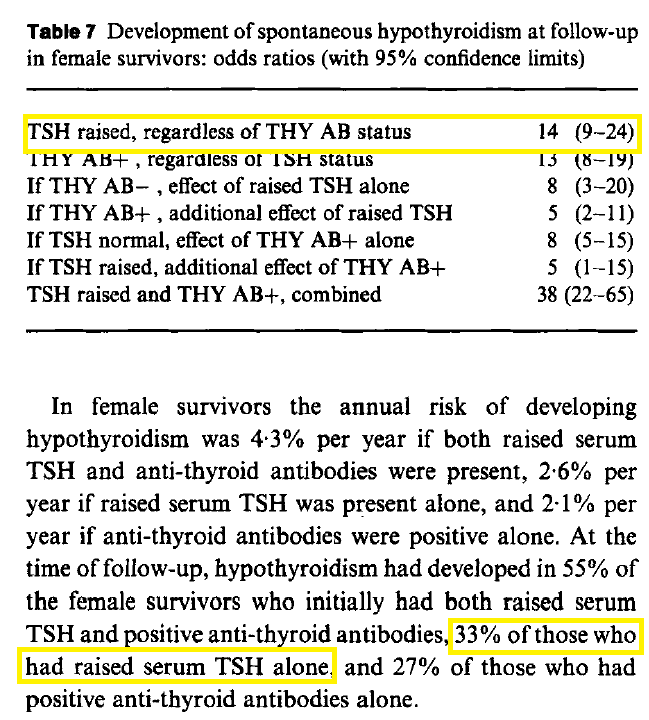
Twenty-year Follow-up of the Whickham Survey
The Whickham Survey carried out between 1972 and 1974 examined the prevalence of thyroid disorders in a randomly selected sample of 2779 adults typical of the general population. The follow-up study published in 1995 established the incidence of thyroid disorders during the period along with the odds ratios of developing thyroid disease and the influence of factors such as TSH levels. As can be seen below subjects with an elevated TSH were 14 times more likely to develop primary hypothyroidism, the odds were much higher for men but on a smaller scale. After 20 years 55% and 33% of women with an elevated TSH (with and without antibodies) developed hypothyroidism.
People with higher TSH levels are more likely to develop hypothyroidism and receive levothyroxine therapy which might be associated with increased cancer risk (see next section). Thus, those with a lower fT4 (higher TSH) at baseline are more likely to have a higher fT4 during the study period! Furthermore, cancer is more prevalent in the elderly, a group who are also more likely to be hypothyroid thus increasing the bias.
Summary
Studies in the general population have conflicting results. A fundamental constraint is that people with abnormal fT4 levels are likely to receive treatment and this confounds the analysis. The evidence for a link between fT4 and cancer in the general population is not strong enough for us to come to a definite conclusion. Let’s look at levothyroxine and cancer.